Psychopathology
Main article: Pathophysiology of HIV/AIDS
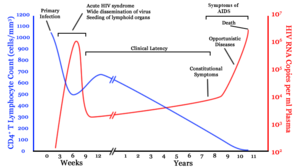
After the virus enters the body there is a period of rapid viral replication, leading to an abundance of virus in the peripheral blood. During primary infection, the level of HIV may reach several million virus particles per milliliter of blood. This response is accompanied by a marked drop in the number of circulating CD4+ T cells. The acute viremia is almost invariably associated with activation of CD8+ T cells, which kill HIV-infected cells, and subsequently with antibody production, orseroconversion. The CD8+ T cell response is thought to be important in controlling virus levels, which peak and then decline, as the CD4+ T cell counts recover. A good CD8+ T cell response has been linked to slower disease progression and a better prognosis, though it does not eliminate the virus.
Ultimately, HIV causes AIDS by depleting CD4+ T ce. This weakens the immune system and allows opportunistic infections. T cells are essential to the immune response and without them, the body cannot fight infections or kill cancerous cells. The mechanism of CD4+ T cell depletion differs in the acute and chronic phases.During the acute phase, HIV-induced cell lysis and killing of infected cells by cytotoxic T cells accounts for CD4+ T cell depletion, although apoptosis may also be a factor. During the chronic phase, the consequences of generalized immune activation coupled with the gradual loss of the ability of the immune system to generate new T cells appear to account for the slow decline in CD4+ T cell numbers.
Although the symptoms of immune deficiency characteristic of AIDS do not appear for years after a person is infected, the bulk of CD4+ T cell loss occurs during the first weeks of infection, especially in the intestinal mucosa, which harbors the majority of the lymphocytes found in the body. The reason for the preferential loss of mucosal CD4+ T cells is that the majority of mucosal CD4+ T cells express the CCR5 protein which HIV uses as a co-receptor to gain access to the cells, whereas only a small fraction of CD4+ T cells in the bloodstream do so. A specific genetic change that alters the CCR5protein when present in both chromosomes very effectively prevents HIV-1 infection.
HIV seeks out and destroys CCR5 expressing CD4+ T cells during acute infection. A vigorous immune response eventually controls the infection and initiates the clinically latent phase. CD4+ T cells in mucosal tissues remain particularly affected. Continuous HIV replication causes a state of generalized immune activation persisting throughout the chronic phase. Immune activation, which is reflected by the increased activation state of immune cells and release of pro-inflammatory cytokines, results from the activity of several HIV gene products and the immune response to ongoing HIV replication. It is also linked to the breakdown of the immune surveillance system of the gastrointestinal mucosal barrier caused by the depletion of mucosal CD4+ T cells during the acute phase of disease.
Diagnosis
Main article: Diagnosis of HIV/AIDS
HIV/AIDS is diagnosed via laboratory testing and then staged based on the presence of certain signs or symptoms. HIV screening is recommended by the United States Preventive Services Task Force for all people 15 years to 65 years of age including all pregnant women.Additionally testing is recommended for all those at high risk, which includes anyone diagnosed with a sexually transmitted illness. In many areas of the world a third of HIV carriers only discover they are infected at an advanced stage of the disease when AIDS or severe immunodeficiency has become apparent.
HIV testing
Most people infected with HIV develop specific antibodies (i.e.seroconvert) within three to twelve weeks of the initial infection.Diagnosis of primary HIV before seroconversion is done by measuring HIV-RNA or p24 antigen. Positive results obtained by antibody or PCR testing are confirmed either by a different antibody or by PCR.
Antibody tests in children younger than 18 months are typically inaccurate due to the continued presence of maternal antibodies. Thus HIV infection can only be diagnosed by PCR testing for HIV RNA or DNA, or via testing for the p24 antigen. Much of the world lacks access to reliable PCR testing and many places simply wait until either symptoms develop or the child is old enough for accurate antibody testing. In sub-Saharan Africa as of 2007–2009 between 30 and 70% of the population was aware of their HIV status. In 2009, between 3.6 and 42% of men and women in Sub-Saharan countries were tested which represented a significant increase compared to previous years.
Classifications
Two main clinical staging systems are used to classify HIV and HIV-related disease for surveillance purposes: the WHO disease staging system for HIV infection and disease,and the CDC classification system for HIV infection. The CDC's classification system is more frequently adopted in developed countries. Since the WHO's staging system does not require laboratory tests, it is suited to the resource-restricted conditions encountered in developing countries, where it can also be used to help guide clinical management. Despite their differences, the two systems allow comparison for statistical purposes.
The World Health Organization first proposed a definition for AIDS in 1986. Since then, the WHO classification has been updated and expanded several times, with the most recent version being published in 2007. The WHO system uses the following categories:
- Primary HIV infection: May be either asymptomatic or associated with acute retroviral syndrome.
- Stage I: HIV infection is asymptomatic with a CD4+ T cell count (also known as CD4 count) greater than 500 per microlitre (µl or cubic mm) of blood. May include generalized lymph node enlargement.
- Stage II: Mild symptoms which may include minor mucocutaneous manifestations and recurrent upper respiratory tract infections. A CD4 count of less than 500/µl.
- Stage III: Advanced symptoms which may include unexplained chronic diarrhea for longer than a month, severe bacterial infections including tuberculosis of the lung, and a CD4 count of less than 350/µl.
- Stage IV or AIDS: severe symptoms which include toxoplasmosis of the brain, candidiasis of the esophagus, trachea,bronchi or lungs and Kaposi's sarcoma. A CD4 count of less than 200/µl.
The United States Center for Disease Control and Prevention also created a classification system for HIV, and updated it in 2008 and 2014. This system classifies HIV infections based on CD4 count and clinical symptoms, and describes the infection in five groups. In those greater than six years of age it is:
- Stage 0: the time between a negative or indeterminate HIV test followed less than 180 days by a positive test
- Stage 1: CD4 count ≥ 500 cells/µl and no AIDS defining conditions
- Stage 2: CD4 count 200 to 500 cells/µl and no AIDS defining conditions
- Stage 3: CD4 count ≤ 200 cells/µl or AIDS defining conditions
- Unknown: if insufficient information is available to make any of the above classifications
For surveillance purposes, the AIDS diagnosis still stands even if, after treatment, the CD4+ T cell count rises to above 200 per µL of blood or other AIDS-defining illnesses are cured.
Prevention
Main article: Prevention of HIV/AIDS
Sexual contact
Consistent condom use reduces the risk of HIV transmission by approximately 80% over the long term. When condoms are used consistently by a couple in which one person is infected, the rate of HIV infection is less than 1% per year. There is some evidence to suggest that female condoms may provide an equivalent level of protection. Application of a vaginal gel containing tenofovir (a reverse transcriptase inhibitor) immediately before sex seems to reduce infection rates by approximately 40% among African women. By contrast, use of the spermicidenonoxynol-9 may increase the risk of transmission due to its tendency to cause vaginal and rectal irritation.
Circumcision in Sub-Saharan Africa "reduces the acquisition of HIV by heterosexual men by between 38% and 66% over 24 months". Based on these studies, the World Health Organization and UNAIDS both recommended male circumcision as a method of preventing female-to-male HIV transmission in 2007. Whether it protects against male-to-female transmission is disputed and whether it is of benefit in developed countries and among men who have sex with men is undetermined. The International Antiviral Society, however, does recommend for all sexually active heterosexual males and that it be discussed as an option with men who have sex with men. Some experts fear that a lower perception of vulnerability among circumcised men may cause more sexual risk-taking behavior, thus negating its preventive effects.
Programs encouraging sexual abstinence do not appear to affect subsequent HIV risk. Evidence for a benefit from peer education is equally poor. Comprehensive sexual education provided at school may decrease high risk behavior. A substantial minority of young people continues to engage in high-risk practices despite knowing about HIV/AIDS, underestimating their own risk of becoming infected with HIV. Voluntary counseling and testing people for HIV does not affect risky behavior in those who test negative but does increase condom use in those who test positive. It is not known whether treating other sexually transmitted infections is effective in preventing HIV.
Pre-exposure
Treating people with HIV whose CD4 count ≥ 350cells/µL with antiretrovirals protects 96% of their partners from infection. This is about a 10 to 20 fold reduction in transmission risk. Pre-exposure prophylaxis (PrEP) with a daily dose of the medications tenofovir, with or without emtricitabine, is effective in a number of groups including men who have sex with men, couples where one is HIV positive, and young heterosexuals in Africa. It may also be effective in intravenous drug users with a study finding a decrease in risk of 0.7 to 0.4 per 100 person years.
Universal precautions within the health care environment are believed to be effective in decreasing the risk of HIV.Intravenous drug use is an important risk factor and harm reduction strategies such as needle-exchange programmes andopioid substitution therapy appear effective in decreasing this risk.
Post-exposure
A course of antiretrovirals administered within 48 to 72 hours after exposure to HIV-positive blood or genital secretions is referred to as post-exposure prophylaxis (PEP). The use of the single agent zidovudine reduces the risk of a HIV infection five-fold following a needle-stick injury. As of 2013, the prevention regimen recommended in the United States consists of three medications—tenofovir, emtricitabine and raltegravir—as this may reduce the risk further.
PEP treatment is recommended after a sexual assault when the perpetrator is known to be HIV positive, but is controversial when their HIV status is unknown. The duration of treatment is usually four weeks and is frequently associated with adverse effects—where zidovudine is used, about 70% of cases result in adverse effects such as nausea (24%), fatigue (22%), emotional distress (13%) and headaches (9%).
Mother-to-child
Main article: HIV and pregnancy
Programs to prevent the vertical transmission of HIV (from mothers to children) can reduce rates of transmission by 92–99%. This primarily involves the use of a combination of antiviral medications during pregnancy and after birth in the infant and potentially includes bottle feeding rather than breastfeeding.If replacement feeding is acceptable, feasible, affordable, sustainable, and safe, mothers should avoid breastfeeding their infants; however exclusive breastfeeding is recommended during the first months of life if this is not the case. If exclusive breastfeeding is carried out, the provision of extended antiretroviral prophylaxis to the infant decreases the risk of transmission.
Vaccination
Main article: HIV vaccine
As of 2012 there is no effective vaccine for HIV or AIDS. A single trial of the vaccine RV 144 published in 2009 found a partial reduction in the risk of transmission of roughly 30%, stimulating some hope in the research community of developing a truly effective vaccine. Further trials of the RV 144 vaccine are ongoing.
Treatment
Main article: Management of HIV/AIDS
There is currently no cure or effective HIV vaccine. Treatment consists of highly active antiretroviral therapy (HAART) which slows progression of the disease. As of 2010 more than 6.6 million people were taking them in low and middle income countries. Treatment also includes preventive and active treatment of opportunistic infections.
Antiviral therapy
Current HAART options are combinations (or "cocktails") consisting of at least three medications belonging to at least two types, or "classes," of antiretroviral agents.Initially treatment is typically a non-nucleoside reverse transcriptase inhibitor(NNRTI) plus two nucleoside analogue reverse transcriptase inhibitors (NRTIs).[132]Typical NRTIs include: zidovudine (AZT) or tenofovir (TDF) and lamivudine (3TC) oremtricitabine (FTC). Combinations of agents which include protease inhibitors(PI) are used if the above regimen loses effectiveness.
When to start antiretroviral therapy is subject to debate. The World Health Organization recommends antiretrovirals in all adolescents, adults and pregnant women with a CD4 count less than 500/µl with this being especially important in those with counts less than 350/µl or those with symptoms regardless of CD4 count. This is supported by the fact that beginning treatment at this level reduces the risk of death. The United States in addition recommends them for all HIV-infected people regardless of CD4 count or symptoms; however it makes this recommendation with less confidence for those with higher counts.[ While the WHO also recommends treatment in those who are co-infected with tuberculosis and those with chronic active hepatitis B. Once treatment is begun it is recommended that it is continued without breaks or "holidays". Many people are diagnosed only after treatment ideally should have begun. The desired outcome of treatment is a long term plasma HIV-RNA count below 50 copies/mL.Levels to determine if treatment is effective are initially recommended after four weeks and once levels fall below 50 copies/mL checks every three to six months are typically adequate. Inadequate control is deemed to be greater than 400 copies/mL. Based on these criteria treatment is effective in more than 95% of people during the first year.
Benefits of treatment include a decreased risk of progression to AIDS and a decreased risk of death. In the developing world treatment also improves physical and mental health. With treatment there is a 70% reduced risk of acquiring tuberculosis. Additional benefits include a decreased risk of transmission of the disease to sexual partners and a decrease in mother-to-child transmission. The effectiveness of treatment depends to a large part on compliance.Reasons for non-adherence include poor access to medical care, inadequate social supports, mental illness and drug abuse.The complexity of treatment regimens (due to pill numbers and dosing frequency) and adverse effects may reduce adherence. Even though cost is an important issue with some medications,47% of those who needed them were taking them in low and middle income countries as of 2010 and the rate of adherence is similar in low-income and high-income countries.
Specific adverse events are related to the antiretroviral agent taken. Some relatively common adverse events include:lipodystrophy syndrome, dyslipidemia, and diabetes mellitus, especially with protease inhibitors. Other common symptoms include diarrhea,and an increased risk of cardiovascular disease Newer recommended treatments are associated with fewer adverse effects. Certain medications may be associated with birth defects and therefore may be unsuitable for women hoping to have children.
Treatment recommendations for children are somewhat different from those for adults. The World Health Organisation recommends treating all children less than 5 years of age; children above 5 are treated like adults. The United States guidelines recommend treating all children less than 12 months of age and all those with HIV RNA counts greater than 100,000 copies/mL between one year and five years of age.
Opportunistic infections
Measures to prevent opportunistic infections are effective in many people with HIV/AIDS. In addition to improving current disease, treatment with antiretrovirals reduces the risk of developing additional opportunistic infections.Adults and adolescents who are living with HIV (even on anti-retroviral therapy) with no evidence of active tuberculosis in settings with high tuberculosis burden should receive isoniazid preventive therapy (IPT), the tuberculin skin test can be used to help decide if IPT is needed. Vaccination against hepatitis A and B is advised for all people at risk of HIV before they become infected; however it may also be given after infection. Trimethoprim/sulfamethoxazole prophylaxis between four and six weeks of age and ceasing breastfeeding in infants born to HIV positive mothers is recommended in resource limited settings. It is also recommended to prevent PCP when a person's CD4 count is below 200 cells/uL and in those who have or have previously had PCP. People with substantial immunosuppression are also advised to receive prophylactic therapy for toxoplasmosis and Cryptococcus meningitis. Appropriate preventive measures have reduced the rate of these infections by 50% between 1992 and 1997.
Diet
Main article: Nutrition and HIV/AIDS
The World Health Organization (WHO) has issued recommendations regarding nutrient requirements in HIV/AIDS. A generally healthy diet is promoted. Some evidence has shown a benefit from micronutrient supplements. Evidence for supplementation with selenium is mixed with some tentative evidence of benefit. There is some evidence that vitamin Asupplementation in children reduces mortality and improves growth. In Africa in nutritionally compromised pregnant and lactating women a multivitamin supplementation has improved outcomes for both mothers and children.Dietary intake of micronutrients at RDA levels by HIV-infected adults is recommended by the WHO; higher intake of vitamin A, zinc, and iron can produce adverse effects in HIV positive adults, and is not recommended unless there is documented deficiency.
Alternative medicine
In the US, approximately 60% of people with HIV use various forms of complementary or alternative medicine,even though the effectiveness of most of these therapies has not been established.There is not enough evidence to support the use of herbal medicines.There is insufficient evidence to recommend or support the use of medical cannabis to try to increase appetite or weight gain.
Prognosis
HIV/AIDS has become a chronic rather than an acutely fatal disease in many areas of the world.Prognosis varies between people, and both the CD4 count and viral load are useful for predicted outcomes. Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype. After the diagnosis of AIDS, if treatment is not available, survival ranges between 6 and 19 months. HAART and appropriate prevention of opportunistic infections reduces the death rate by 80%, and raises the life expectancy for a newly diagnosed young adult to 20–50 years. This is between two thirds and nearly that of the general population. If treatment is started late in the infection, prognosis is not as good: for example, if treatment is begun following the diagnosis of AIDS, life expectancy is ~10–40 years. Half of infants born with HIV die before two years of age without treatment.
The primary causes of death from HIV/AIDS are opportunistic infections andcancer, both of which are frequently the result of the progressive failure of the immune system.Risk of cancer appears to increase once the CD4 count is below 500/μL The rate of clinical disease progression varies widely between individuals and has been shown to be affected by a number of factors such as a person's susceptibility and immune function; their access to health care, the presence of co-infections; and the particular strain (or strains) of the virus involved.
Tuberculosis co-infection is one of the leading causes of sickness and death in those with HIV/AIDS being present in a third of all HIV infected people and causing 25% of HIV related deaths. HIV is also one of the most important risk factors for tuberculosis. Hepatitis C is another very common co-infection where each disease increases the progression of the other. The two most common cancers associated with HIV/AIDS are Kaposi's sarcoma and AIDS-related non-Hodgkin's lymphoma.
Even with anti-retroviral treatment, over the long term HIV-infected people may experience neurocognitive disorders,]osteoporosis, neuropathy, cancers, nephropathy and cardiovascular disease. Some conditions likelipodystrophy may be caused both by HIV and its treatment
Epidemiology
Main article: Epidemiology of HIV/AIDS
HIV/AIDS is a global As of 2012, approximately 35.3 million people have HIV worldwide with the number of new infections that year being about 2.3 million. This is down from 3.1 million new infections in 2001.Of these approximately 16.8 million are women and 3.4 million are less than 15 years old. It resulted in about 1.34 million deaths in 2013, down from a peak of 2.2 million in 2005.
Sub-Saharan Africa is the region most affected. In 2010, an estimated 68% (22.9 million) of all HIV cases and 66% of all deaths (1.2 million) occurred in this region. This means that about 5% of the adult population is infected and it is believed to be the cause of 10% of all deaths in children. Here in contrast to other regions women compose nearly 60% of cases. South Africa has the largest population of people with HIV of any country in the world at 5.9 million. Life expectancy has fallen in the worst-affected countries due to HIV/AIDS; for example, in 2006 it was estimated that it had dropped from 65 to 35 years in Botswana. Mother-to-child transmission, as of 2013, in Botswana and South Africa has decreased to less than 5% with improvement in many other African nations due to improved access to antiretroviral therapy.
South & South East Asia is the second most affected; in 2010 this region contained an estimated 4 million cases or 12% of all people living with HIV resulting in approximately 250,000 deaths.Approximately 2.4 million of these cases are in India.
In 2008 in the United States approximately 1.2 million people were living with HIV, resulting in about 17,500 deaths. The US Centers for Disease Control and Prevention estimated that in 2008 20% of infected Americans were unaware of their infection. In the United Kingdom as of 2009 there where approximately 86,500 cases which resulted in 516 deaths.In Canada as of 2008 there were about 65,000 cases causing 53 deaths. Between the first recognition of AIDS in 1981 and 2009 it has led to nearly 30 million deaths.Prevalence is lowest in Middle East and North Africa at 0.1% or less,East Asia at 0.1% and Western and Central Europe at 0.2%.The worst affected European countries, in 2009 and 2012 estimates, are Russia, Ukraine, Latvia, Moldova, Portugal and Belarus, in order of prevalence.
History
Main article: History of HIV/AIDS
Discovery
AIDS was first clinically observed in 1981 in the United States. The initial cases were a cluster of injecting drug users and homosexual men with no known cause of impaired immunity who showed symptoms of Pneumocystis carinii pneumonia (PCP), a rare opportunistic infection that was known to occur in people with very compromised immune systems. Soon thereafter, an unexpected number of homosexual men developed a previously rare skin cancer called Kaposi's sarcoma(KS). Many more cases of PCP and KS emerged, alerting U.S. Centers for Disease Control and Prevention (CDC) and a CDC task force was formed to monitor the outbreak.
In the early days, the CDC did not have an official name for the disease, often referring to it by way of the diseases that were associated with it, for example,lymphadenopathy, the disease after which the discoverers of HIV originally named the virus. They also used Kaposi's sarcoma and opportunistic infections, the name by which a task force had been set up in 1981. At one point, the CDC coined the phrase "the 4H disease", since the syndrome seemed to affect homosexuals, heroin users, hemophiliacs, and Haitians. In the general press, the term "GRID", which stood for gay-related immune deficiency, had been coined. However, after determining that AIDS was not isolated to the gay community, it was realized that the term GRID was misleading and the term AIDS was introduced at a meeting in July 1982 By September 1982 the CDC started referring to the disease as AIDS.
In 1983, two separate research groups led by Robert Gallo and Luc Montagnier independently declared that a novel retrovirus may have been infecting people with AIDS, and published their findings in the same issue of the journalScience. Gallo claimed that a virus his group had isolated from a person with AIDS was strikingly similar in shape to other human T-lymphotropic viruses (HTLVs) his group had been the first to isolate. Gallo's group called their newly isolated virus HTLV-III. At the same time, Montagnier's group isolated a virus from a person presenting with swelling of thelymph nodes of the neck and physical weakness, two characteristic symptoms of AIDS. Contradicting the report from Gallo's group, Montagnier and his colleagues showed that core proteins of this virus were immunologically different from those of HTLV-I. Montagnier's group named their isolated virus lymphadenopathy-associated virus (LAV). As these two viruses turned out to be the same, in 1986, LAV and HTLV-III were renamed HIV.
Origins
Both HIV-1 and HIV-2 are believed to have originated in non-humanprimates in West-central Africa and were transferred to humans in the early 20th century. HIV-1 appears to have originated in southernCameroon through the evolution of SIV(cpz), a simian immunodeficiency virus (SIV) that infects wild chimpanzees (HIV-1 descends from the SIVcpz endemic in the chimpanzee subspecies Pan troglodytes troglodytes). The closest relative of HIV-2 is SIV(smm), a virus of the sooty mangabey (Cercocebus atys atys), an Old World monkey living in coastal West Africa (from southern Senegalto western Côte d'Ivoire). New World monkeys such as the owl monkey are resistant to HIV-1 infection, possibly because of a genomic fusion of two viral resistance genes. HIV-1 is thought to have jumped the species barrier on at least three separate occasions, giving rise to the three groups of the virus, M, N, and O.
There is evidence that humans who participate in bushmeat activities, either as hunters or as bushmeat vendors, commonly acquire SI. However, SIV is a weak virus which is typically suppressed by the human immune system within weeks of infection. It is thought that several transmissions of the virus from individual to individual in quick succession are necessary to allow it enough time to mutate into HIV.Furthermore, due to its relatively low person-to-person transmission rate, SIV can only spread throughout the population in the presence of one or more high-risk transmission channels, which are thought to have been absent in Africa before the 20th century.
Specific proposed high-risk transmission channels, allowing the virus to adapt to humans and spread throughout the society, depend on the proposed timing of the animal-to-human crossing. Genetic studies of the virus suggest that the most recent common ancestor of the HIV-1 M group dates back to circa 1910. Proponents of this dating link the HIV epidemic with the emergence of colonialism and growth of large colonial African cities, leading to social changes, including a higher degree of sexual promiscuity, the spread of prostitution, and the accompanying high frequency of genital ulcer diseases(such as syphilis) in nascent colonial cities.While transmission rates of HIV during vaginal intercourse are low under regular circumstances, they are increased many fold if one of the partners suffers from a sexually transmitted infectioncausing genital ulcers. Early 1900s colonial cities were notable due to their high prevalence of prostitution and genital ulcers, to the degree that, as of 1928, as many as 45% of female residents of eastern Kinshasa were thought to have been prostitutes, and, as of 1933, around 15% of all residents of the same city had syphilis.
An alternative view holds that unsafe medical practices in Africa after World War II, such as unsterile reuse of single use syringes during mass vaccination, antibiotic and anti-malaria treatment campaigns, were the initial vector that allowed the virus to adapt to humans and spread.
The earliest well documented case of HIV in a human dates back to 1959 in the Congo. The virus may have been present in the United States as early as 1966, but the vast majority of infections occurring outside sub-Saharan Africa (including the U.S.) can be traced back to a single unknown individual who became infected with HIV in Haiti and then brought the infection to the United States some time around 1969. The epidemic then rapidly spread among high-risk groups (initially, sexually promiscuous men who have sex with men). By 1978, the prevalence of HIV-1 among homosexual male residents of New York and San Francisco was estimated at 5%, suggesting that several thousand individuals in the country had been infected.



















Most prostate cancers are adenocarcinomas, cancers that arise in glandular cells of the prostate’s epithelial tissue. Prostate cancers usually progress slowly and produce no symptoms in the initial stages. Eventually, the tumor may enlarge like mine use too, the prostate gland, pressing on the urethra and causing painful or frequent urination and blood in the urine. So I was so uncomfortable with this prostate cancer diseases then I decided to do online search on how to cure cancer because I well have read a lot about herbal medicine, I came across a lot of testimony how Dr Itua cure HIV/herpes then Cancer was listed below the comment.with courage I contacted Dr Itua and he sent me his herbal medicine through Courier service then I was asked to pick it up at my post office which i quickly did. I contacted Dr Itua that i have received my herbal medicine so he instructs me on how to drink it for three weeks and that is how Dr Itua Herbal Medicine cure my prostate Cancer, The treatment takes three weeks and I was cured completely. Dr Itua is a god sent and I thank him every day of my life. Contact him now On:Email:drituaherbalcenter@gmail.com/ Whatsapp:+2348149277967.
ReplyDeleteHe listed to that he can as well cure the following diseases below.... Cerebral Amides. Lung Cancer,Brain cancer,Esophageal cancer,Gallbladder cancer,Gestational trophoblastic disease,Head and neck cancer,Hodgkin lymphoma Intestinal cancer,Kidney cancer,Leukemia,Liver cancer,Melanoma,Mesothelioma,Multiple myeloma,Neuroendocrine tumors,Hodgkin lymphoma,Oral cancer,Ovarian cancer,Sinus cancer,Soft tissue sarcoma,Spinal cancer,Stomach cancer,Meniere's disease , Testicular cancer,Throat cancer,Thyroid Cancer,Uterine cancer,Vaginal cancer,Vulvar cancer. Alzheimer's disease,Autism,measles, tetanus, whooping cough, tuberculosis, polio and diphtheria Adrenocortical carcinoma. Alma, Uterine Cancer, Breast Cancer, Allergic diseases. Kidney cancer, Love Spell, Glaucoma., Cataracts,Macular degeneration,Cardiovascular disease,Lung disease.Enlarged prostate,Osteoporosis.Generalized dermatitis,Alzheimer's disease,Brain Tumor,Lupus,Endomertil Cancer, cerebrovascular diseases
Dementia.Colo rectal cancer, Lottery Spell, Bladder Cancer, Skin Cancer,Ovarian Cancer,Pancreatic Cancer, HIV /Aids,Brain Tumor, Herpes, Non-Hodgkin lymphoma, Inflammatory bowel disease, Copd, Diabetes, Hepatitis
Great Dr. imoloa herbal medicine is the perfect cure for the HIV virus, I was diagnosed of HIV for 8 years, and every day I always looking for research to find the perfect way to get rid of this terrible disease because I always know that what we need because our health is on earth . So, on my internet search I saw several testimonies about how Dr. imoloa can cure HIV with powerful herbal medicines. I decided to contact this man, I contacted him for herbal medicines that I received via DHL courier service. And he guided me how. I asked him for a solution to take herbal medicine for two weeks. And then he instructed me to go check what I was doing. Look at me (HIV NEGATIVE). Thank God for Dr. Imoloa for using a powerful herbal remedy to cure me. he also has a cure for diseases such as Parkison's disease, vaginal cancer, epilepsy, anxiety disorders, autoimmune diseases, back pain, sprains, bipolar disorder, brain tumors, malignant, bruxism, bulimia, cervical disc disease, cardiovascular disease, cardiovascular disease, sprains, bipolar disorder, brain tumors, malignant, bruxism, bulimia, cervical disc disease, cardiovascular disease, cardiovascular disease, sprains, bipolar disorder, brain tumors, malignant, bruxism, bulimia, cervical disc disease, cardiovascular disease , chronic respiratory diseases, mental and behavioral disorders, Cystic Fibrosis, Hypertension, Diabetes, asthma, autoimmune mediated arthritis. Chronic kidney disease, arthritis, back pain, impotence, feta alcohol spectrum, Dysthymic Disorders, Eczema, skin cancer, tuberculosis, Chronic Fatigue Syndrome, constipation, inflammatory bowel disease, bone cancer, lung cancer, mouth sores, oral cancer, body pain, fever, hepatitis ABC, syphilis, diarrhea, Huntington's disease, back acne, chronic kidney failure, Addison's disease, Chronic Disease, Crohn's Disease, Cystic Fibrosis, Fibromyalgia, Inflammatory Bowel Disease, Fungal Nail Disease, Paralysis, Celia Disease , Lymphoma, Major Depression, Malignant Melanoma, Mania, Melorheostosis, Meniere's Disease, Mucopolysaccharidosis, Multiple Sclerosis, Muscle Dystrophy, Rheumatoid Arthritis, Alzheimer's Disease email- drimolaherbalmademedicine@gmail.com / or {whatssapp .....+2347081986098}
ReplyDeleteI thought my life had become meaningless and had nothing to offer anymore as I had HIV, the symptoms became very severe and bold which made my family and friends run away from me and abandoned me, so they won't get infected. I gave up everything, my hope, dreams, vision and job because doctors told me there's no cure. I consumed so many antiviral drugs, but they never cured me but hid the symptoms inside me, It was worse. I was desperate to find a solution to this horrible and deadly virus inside me. I made online research on herbal remedy for HIV/Aids cure when I came across testimonies of some people on how DR JAMES uses his herbal mix medicine to Cured them of MENINGITIS, DENGUE, SCHIZOPHRENIA, BIPOLAR DISORDER, ALZHEIMER'S DISEASES, UNDERACTIVE THYROID, HIV/AIDS. HERPES VIRUS. CANCER, ALS, STROKE, HEPATITIS B, DIABETES, FIBROID, MULTIPLE SCLEROSIS, CARDIOVASCULAR DISEASES, LUPUS, SKIN CANCER.OVARIAN CANCER, I never believed at first and thought it was a joke but later decided to contact him on the details provided and when I messaged him we talked, and he told me on how his herbs and root medicine works Which was all okay with me. He sent me his herbal mix medicine and told me the usage and I should go for a test after 3 weeks of drinking the herbal medicine Within 7 days of his medications the symptoms disappeared and when I went for a test Lo and behold I negative by the Doctor Who tested me earlier. Thank you DR James for saving my life and I'll keep telling the world about you. If you're out there going through pains, rejection and facing any kind of health challenges Worry no more and contact DR James via.GREATCUREMAN@GMAIL.COM / INFO@DRJAMESHERBALMIX@GMAIL.COM He's a good man, and he will surely help you.
ReplyDelete