HIV/AIDS
Human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV). Following initial infection, a person may experience a brief period of influenza-like illness. This is typically followed by a prolonged period without symptoms. As the infection progresses, it interferes more and more with the immune system, making the person much more susceptible to common infections like tuberculosis, as well as opportunistic infections and tumors that do not usually affect people who have working immune systems. The late symptoms of the infection are referred to as AIDS. This stage is often complicated by an infection of the lung known as pneumocystis pneumonia, severe weight loss, a type of cancer known as Kaposi's sarcoma, or other AIDS-defining conditions.
HIV is transmitted primarily via unprotected sexual intercourse (including analand oral sex), contaminated blood transfusions, hypodermic needles, and from mother to child during pregnancy, delivery, or breastfeeding. Some bodily fluids, such as saliva and tears, do not transmit HIV. Common methods ofHIV/AIDS prevention include encouraging safe sex, needle-exchange programs, and treating those who are infected.There is no cure or vaccine; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy. While antiretroviral treatment reduces the risk of death and complications from the disease, these medications are expensive and have side effects. Without treatment, the average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype.
Since its discovery, AIDS has caused an estimated 36 million deaths worldwide (as of 2012). In 2013 it resulted in about 1.34 million deaths. As of 2012, approximately 35.3 million people are living with HIV globally. HIV/AIDS is considered apandemic—a disease outbreak which is present over a large area and is actively spreading. Genetic research indicates that HIV originated in west-central Africa during the late nineteenth or early twentieth century. AIDS was first recognized by the United States Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade.
HIV/AIDS has had a great impact on society, both as an illness and as a source of discrimination. The disease also has significant economic impacts. There are many misconceptions about HIV/AIDS such as the belief that it can be transmitted by casual non-sexual contact. The disease has become subject to many controversies involving religion. It has attracted international medical and political attention as well as large-scale funding since it was identified in the 1980s.
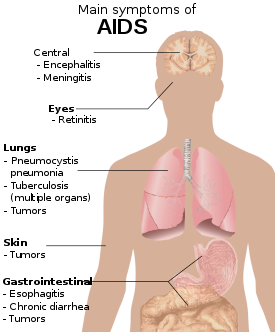
Signs and symptoms
Main article: Signs and symptoms of HIV/AIDS
There are three main stages of HIV infection: acute infection, clinical latency and AIDS.
Acute infection
The initial period following the contraction of HIV is called acute HIV, primary HIV or acute retroviral syndrome. Many individuals develop an influenza-like illness or a mononucleosis-like illness 2–4 weeks post exposure while others have no significant symptoms. Symptoms occur in 40–90% of cases and most commonly include fever, large tender lymph nodes, throat inflammation, a rash, headache, and/or sores of the mouth and genitals. The rash, which occurs in 20–50% of cases, presents itself on the trunk and is maculopapular, classically. Some people also develop opportunistic infections at this stage.Gastrointestinal symptoms such as nausea, vomiting or diarrhea may occur, as may neurological symptoms of peripheral neuropathy or Guillain-Barre syndrome. The duration of the symptoms varies, but is usually one or two weeks.
Due to their nonspecific character, these symptoms are not oftenrecognized as signs of HIV infection. Even cases that do get seen by a family doctor or a hospital are often misdiagnosed as one of the many common infectious diseases with overlapping symptoms. Thus, it is recommended that HIV be considered in people presenting an unexplained fever who may have risk factors for the infection.
Clinical latency
The initial symptoms are followed by a stage called clinical latency, asymptomatic HIV, or chronic HIV. Without treatment, this second stage of the natural history of HIV infection can last from about three years to over 20 years (on average, about eight years). While typically there are few or no symptoms at first, near the end of this stage many people experience fever, weight loss, gastrointestinal problems and muscle pains. Between 50 and 70% of people also developpersistent generalized lymphadenopathy, characterized by unexplained, non-painful enlargement of more than one group of lymph nodes (other than in the groin) for over three to six months.
Although most HIV-1 infected individuals have a detectable viral load and in the absence of treatment will eventually progress to AIDS, a small proportion (about 5%) retain high levels of CD4+ T cells (T helper cells) without antiretroviral therapy for more than 5 years.These individuals are classified as HIV controllers or long-term nonprogressors(LTNP). Another group is those who also maintain a low or undetectable viral load without anti-retroviral treatment who are known as "elite controllers" or "elite suppressors". They represent approximately 1 in 300 infected persons.
Acquired immunodeficiency syndrome
Acquired immunodeficiency syndrome (AIDS) is defined in terms of either a CD4+ T cell count below 200 cells per µL or the occurrence of specific diseases in association with an HIV infection. In the absence of specific treatment, around half of people infected with HIV develop AIDS within ten years. The most common initial conditions that alert to the presence of AIDS are pneumocystis pneumonia (40%), cachexia in the form of HIV wasting syndrome (20%) and esophageal candidiasis. Other common signs include recurring respiratory tract infections.
Opportunistic infections may be caused by bacteria, viruses, fungi andparasites that are normally controlled by the immune system. Which infections occur partly depends on what organisms are common in the person's environment. These infections may affect nearly every organ system.
People with AIDS have an increased risk of developing various viral induced cancers including Kaposi's sarcoma, Burkitt's lymphoma, primary central nervous system lymphoma and cervical cancer. Kaposi's sarcoma is the most common cancer occurring in 10 to 20% of people with HIV. The second most common cancer is lymphoma which is the cause of death of nearly 16% of people with AIDS and is the initial sign of AIDS in 3 to 4%. Both these cancers are associated with human herpesvirus 8. Cervical cancer occurs more frequently in those with AIDS due to its association with human papillomavirus (HPV). Conjunctival cancer(of the layer which lines the inner part of eyelids and the white part of the eye) is more common in those with HIV.
Additionally, people with AIDS frequently have systemic symptoms such as prolonged fevers, sweats (particularly at night), swollen lymph nodes, chills, weakness, and unintended weight loss. Diarrhea is another common symptom present in about 90% of people with AIDS. They can also be affected by diverse psychiatric and neurological symptoms independent of opportunistic infections and cancers.
Transmission
| Exposure route | Chance of infection | |||
|---|---|---|---|---|
| Blood transfusion | 90% | |||
| Childbirth (to child) | 25% | |||
| Needle-sharing injection drug use | 0.67% | |||
| Percutaneous needle stick | 0.30% | |||
| Receptive anal intercourse* | 0.04–3.0% | |||
| Insertive anal intercourse* | 0.03% | |||
| Receptive penile-vaginal intercourse* | 0.05–0.30% | |||
| Insertive penile-vaginal itercourse* | 0.01–0.38% | |||
| Receptive oral interconurse*§ | 0–0.04% | |||
| Insertive oral intercourse*§ | 0–0.005% | |||
| * assuming no condom use § source refers to oral intercourse performed on a man | ||||
HIV is transmitted by three main routes: sexual contact, exposure to infected body fluids or tissues, and from mother to child during pregnancy, delivery, or breastfeeding (known asvertical transmission). There is no risk of acquiring HIV if exposed to feces, nasal secretions, saliva, sputum, sweat, tears, urine, or vomit unless these are contaminated with blood. It is possible to be co-infected by more than one strain of HIV—a condition known as HIV superinfection.
Sexual
The most frequent mode of transmission of HIV is through sexual contact with an infected person. The majority of all transmissions worldwide occur through heterosexual contacts (i.e. sexual contacts between people of the opposite sex);however, the pattern of transmission varies significantly among countries. In the United States, as of 2009, most sexual transmission occurred in men who had sex with men, with this population accounting for 64% of all new cases.
With regard to unprotected heterosexual contacts, estimates of the risk of HIV transmission per sexual act appear to be four to ten times higher in low-income countries than in high-income countries. In low-income countries, the risk of female-to-male transmission is estimated as 0.38% per act, and of male-to-female transmission as 0.30% per act; the equivalent estimates for high-income countries are 0.04% per act for female-to-male transmission, and 0.08% per act for male-to-female transmission. The risk of transmission from anal intercourse is especially high, estimated as 1.4–1.7% per act in both heterosexual and homosexual contacts. While the risk of transmission from oral sex is relatively low, it is still present. The risk from receiving oral sex has been described as "nearly nil"; however, a few cases have been reported. The per-act risk is estimated at 0–0.04% for receptive oral intercourse. In settings involving prostitution in low income countries, risk of female-to-male transmission has been estimated as 2.4% per act and male-to-female transmission as 0.05% per act.
Risk of transmission increases in the presence of many sexually transmitted infections and genital ulcers.Genital ulcers appear to increase the risk approximately fivefold. Other sexually transmitted infections, such as gonorrhea,chlamydia, trichomoniasis, and bacterial vaginosis, are associated with somewhat smaller increases in risk of transmission.
The viral load of an infected person is an important risk factor in both sexual and mother-to-child transmission. During the first 2.5 months of an HIV infection a person's infectiousness is twelve times higher due to this high viral load. If the person is in the late stages of infection, rates of transmission are approximately eightfold greater.
Commercial sex workers (including those in pornography) have an increased rate of HIV. Rough sex can be a factor associated with an increased risk of transmission. Sexual assault is also believed to carry an increased risk of HIV transmission as condoms are rarely worn, physical trauma to the vagina or rectum is likely, and there may be a greater risk of concurrent sexually transmitted infections.
Body fluids
The second most frequent mode of HIV transmission is via blood and blood products. Blood-borne transmission can be through needle-sharing during intravenous drug use, needle stick injury, transfusion of contaminated blood or blood product, or medical injections with unsterilised equipment. The risk from sharing a needle during drug injection is between 0.63 and 2.4% per act, with an average of 0.8%. The risk of acquiring HIV from a needle stick from an HIV-infected person is estimated as 0.3% (about 1 in 333) per act and the risk followingmucous membrane exposure to infected blood as 0.09% (about 1 in 1000) per act. In the United States intravenous drug users made up 12% of all new cases of HIV in 2009 and in some areas more than 80% of people who inject drugs are HIV positive.
HIV is transmitted in about 93% of blood transfusions using infected blood. In developed countries the risk of acquiring HIV from a blood transfusion is extremely low (less than one in half a million) where improved donor selection and HIV screening is performed; for example, in the UK the risk is reported at one in five million and in the United States it was one in 1.5 million in 2008. In low income countries, only half of transfusions may be appropriately screened (as of 2008),and it is estimated that up to 15% of HIV infections in these areas come from transfusion of infected blood and blood products, representing between 5% and 10% of global infections.
Unsafe medical injections play a significant role in HIV spread in sub-Saharan Africa. In 2007, between 12 and 17% of infections in this region were attributed to medical syringe use. The World Health Organization estimates the risk of transmission as a result of a medical injection in Africa at 1.2%. Significant risks are also associated with invasive procedures, assisted delivery, and dental care in this area of the world.
People giving or receiving tattoos, piercings, and scarification are theoretically at risk of infection but no confirmed cases have been documented. It is not possible for mosquitoes or other insects to transmit HIV.
Mother-to-child
Main articles: HIV and pregnancy and HIV and breastfeeding
HIV can be transmitted from mother to child during pregnancy, during delivery, or through breast milk. This is the third most common way in which HIV is transmitted globally. In the absence of treatment, the risk of transmission before or during birth is around 20% and in those who also breastfeed 35%. As of 2008, vertical transmission accounted for about 90% of cases of HIV in children. With appropriate treatment the risk of mother-to-child infection can be reduced to about 1%. Preventive treatment involves the mother taking antiretrovirals during pregnancy and delivery, an elective caesarean section, avoiding breastfeeding, and administering antiretroviral drugs to the newborn. Antiretrovirals when taken by either the mother or the infant decrease the risk of transmission in those who do breastfeed. Many of these measures are however not available in the developing world. If blood contaminates food during pre-chewing it may pose a risk of transmission.
Virology
Main article: HIV
HIV is the cause of the spectrum of disease known as HIV/AIDS. HIV is aretrovirus that primarily infects components of the human immune systemsuch as CD4 T cells, macrophages and dendritic cells. It directly and indirectly destroys CD4+ T cells.
HIV is a member of the genus Lentivirus, part of the family Retroviridae.Lentiviruses share many morphological and biological characteristics. Many species of mammals are infected by lentiviruses, which are characteristically responsible for long-duration illnesses with a long incubation period.Lentiviruses are transmitted as single-stranded, positive-sense, envelopedRNA viruses. Upon entry into the target cell, the viral RNA genome is converted (reverse transcribed) into double-stranded DNA by a virally encoded reverse transcriptase that is transported along with the viral genome in the virus particle. The resulting viral DNA is then imported into the cell nucleus and integrated into the cellular DNA by a virally encoded integrase and host co-factors. Once integrated, the virus may become latent, allowing the virus and its host cell to avoid detection by the immune system. Alternatively, the virus may be transcribed, producing new RNA genomes and viral proteins that are packaged and released from the cell as new virus particles that begin the replication cycle anew.
HIV is now known to spread between CD4+ T cells by two parallel routes: cell-free spread and cell-to-cell spread, i.e. it employs hybrid spreading mechanisms. In the cell-free spread, virus particles bud from an infected T cell, enter the blood/extracellular fluid and then infect another T cell following a chance encounter. HIV can also disseminate by direct transmission from one cell to another by a process of cell-to-cell spread. The hybrid spreading mechanisms of HIV contribute to the virus's ongoing replication against antiretroviral therapies.
Two types of HIV have been characterized: HIV-1 and HIV-2. HIV-1 is the virus that was originally discovered (and initially referred to also as LAV or HTLV-III). It is more virulent, more infective, and is the cause of the majority of HIV infections globally. The lower infectivity of HIV-2 as compared with HIV-1 implies that fewer people exposed to HIV-2 will be infected per exposure. Because of its relatively poor capacity for transmission, HIV-2 is largely confined to West Africa.















No comments:
Post a Comment